
Two participants from group A and group B had a 10° extension lag. Group A scored 90.38% grip strength compared to the unaffected side, and group B 90.58%. A month later, assessments were performed including: ROM with a goniometer, clinical assessment of rotational deformity in the fifth finger and grip strength of the dominant and non-dominant hands with a Jamar hand dynamometer. 17 After removing the POP and splints, an X-ray was taken, and bone healing clinically assessed with pain present or absent on the fracture line. Group B's management included reducing and immobilising the fourth and fifth fingers in a U-shaped gutter splint with the following joint positions: wrist 30° extension, MCPJ 45° flexed, PIPJs and DIPJs in 15° flexion for a mean of 29.15 days. 17 The management of group A included reduction and immobilisation of the fourth and fifth fingers in a short arm POP with the following joint positions: wrist 30° extension, MCPJ 45° flexed, proximal interphalangeal joints (PIPJs) and distal interphalangeal joints (DIPJs) in 15° flexion for a mean of 29.15 days. The participants were allocated to two groups. The inclusion criteria included sustaining an isolated, extra-articular, neck or shaft fifth metacarpal fracture with more than 30° of angulation. A low GRADE quality of evidence rating was given.

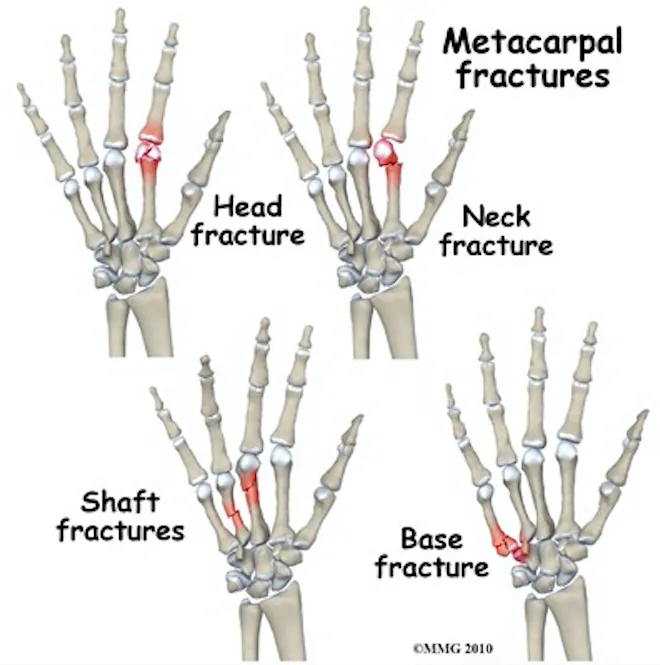
RESULTS: Database searches generated 1 005 articles with ten additional articles found on Google Scholar. Joanna Briggs Institute (jBl) critical appraisal tools were used to assess the risk of bias for each included study. Preferred reporting items for systematic reviews and meta-analysis (PRISMA) guided the reporting. Two reviewers independently screened, selected, appraised and extracted data from the included studies. METHODS: The review included experimental study designs, quasi-experimental studies, cohort studies and case-control studies from January 2008 to September 2018. This review aimed to review, appraise and collate the literature on splints and immobilisation approaches used for second to fifth metacarpal fractures after surgical and conservative management in adults aged 20 to 59 years. However, no recent evidence-based splinting and immobilisation programme exists for the management thereof, leaving a gap in the literature to inform clinical practice. IIIOccupational therapist, private practice, Durban, South AfricaīACKGROUND: The second to fifth metacarpal fractures are immobilised with splints, plaster of Paris (POP) or buddy strapping for a period of time. IIDepartment of Physiotherapy, School of Therapeutic Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa

#3RD METACARPAL FRACTURE SPLINT FREE#
IDepartment of Physiotherapy, School of Health and Rehabilitation Sciences, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa Monique M Keller I, * Roline Y Barnes I Corlia Brandt II Lauren M Hepworth III Splints and immobilisation approaches used for second to fifth metacarpal fractures: a systematic review


 0 kommentar(er)
0 kommentar(er)
